BURRILLVILLE — Jim Whiteside lives about as far into the woods of northwestern Rhode Island as you can go.
Which would not be remarkable until you learn of the multiple health challenges that limit his vision, hearing and mobility.
But thanks to a community health center that makes house calls and provides transportation to office appointments, Whiteside, a retired social worker, remains independent in his home of many years on pristine Wakefield Pond, near Buck Hill.
“A godsend” is how Whiteside describes the center, WellOne Primary Medical and Dental Care, which has offices in Pascoag, Foster, Scituate and North Kingstown.
A cascade of ailments dating back years changed Whiteside’s life.

Anterior ischemic optic neuropathy, more commonly known as optic nerve stroke, stole his vision, although a small degree has returned to one eye. Another condition left him deaf in one ear. A viral infection in his right leg required its amputation. Osteomyelitis has severely damaged his spine. A wheelchair helps get him around.
“I’ve been told that I had a year to live five times,” he said. “I’ve beaten all the odds.”
And he could not have done that, he said, without his rural community health center.
She couldn’t stop one man’s jump.:Now she’s fighting to add suicide barriers to RI bridges
“WellOne has helped every year getting my flu shot, the shingles shot, getting the vaccines for the pandemic,” he said. “It’s much easier to go in town to see the doctors, and they come out here and visit me if I can’t get into town.
“And the dentistry is awesome. I’ve gone in there several times instead of traveling further into the middle of the state, fighting all the traffic. So having something like WellOne in the country has been really great for people like me. They make it much easier. We can go and have our appointments and come back home within an hour.”
‘A special challenge’ in RI’s rural areas
Dr. Michael D. Fine, a former director of the Rhode Island Department of Health who is now the chief health strategist for Central Falls, emphasizes the importance of community health centers throughout Rhode Island — and notes the critical role they play for people like Whiteside.
“People forget how many people, particularly older people and those with disabilities, live in their houses by themselves, which is a special challenge in rural areas, where there is often no doctor’s office nearby,” Fine said. “Community health centers and neighborhood health stations are there for those people.”
While community centers are more common in urban areas, several, like WellOne, provide care to individuals in less-populated regions. Some of the needs of rural residents differ from those of people living in the cities, Fine said, a fact borne out by a 2016 Rhode Island Department of Health study, “Key Determinants of Rural Health in Rhode Island.”
“In rural communities, both in Rhode Island and throughout the United States, low numbers of local health care providers and limited public transportation create barriers to accessing health care,” the study concluded.
A pressing issue is the need for high-quality behavioral health care, according to the study, which noted “for rural residents, who are often socially and geographically isolated and may lack the familial, financial, and community support needed to effectively manage their behavioral health concerns, access to behavioral care specialists is critical.”
In Cranston:Crisis intervention team aligns police officers with behavioral health clinicians
Said Fine, a practicing physician who is himself a patient of WellOne: “Rhode Island’s health centers and neighborhood health stations are critical to our ability to bring personal and affordable health care to all Rhode Islanders — from the centers of our cities to the most isolated and rural of our towns and villages. We need one in every Rhode Island community.”
Born 113 years ago in an epidemic
WellOne has its roots in the early days of the last century, when Rhode Island and America were being punished by the tuberculosis epidemic. What is now the Zambarano unit of state-run Slater Hospital in Pascoag was a sanatorium where many patients perished from a disease that was then incurable.
“On December 21, 1909, as a result of a public meeting and to address the growing threat to the local textile mills, the Burrillville Anti-Tuberculosis Association was founded,” WellOne writes on its website. “Its one employee, nurse Molly Malone, quickly also was caring for other sicknesses and assisting with home-based births and operations.
“Despite a large and rural territory, she tended to all of the villages in Burrillville either by walking” or with house calls made “in a borrowed horse and buggy.”
Today, nonprofit WellOne — which receives some revenue from the state Health Department by means of federal pass-through grants — employs about 150 workers and provides primary care, dental care and behavioral-health services to some 17,000 active patients. Much of this growth has come in the last three decades under the leadership of Peter J. Bancroft, a certified public accountant by training who became chief financial officer in 1992 and has been CEO since 2003, when WellOne’s patient count was about 3,000.
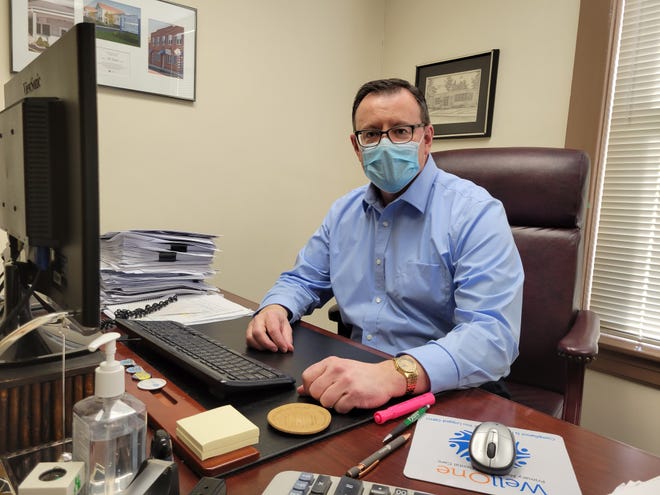
During a recent interview in his downtown Pascoag office, Bancroft said, “from a statistics perspective, about one in four Burrillville residents comes here for health care. Twenty-five percent is a lot.”
COVID-19 pandemic leads to population decline in RI and much of the U.S. Here’s why.
To accommodate them, the Pascoag center has grown from a single small building to a large complex at the corner of Bridge Way and Sayles Avenue. WellOne also rents town-owned space on Main Street, and it recently bought an abandoned bank building at the corner of South Main and Main where behavioral-health services are offered.
“The bank building was sitting there deteriorating,” Bancroft said. “No one was going to come and save it. So we’re a health-care organization, we’re a charitable organization, but I think there’s also a connection and a mission in the community.”
The Foster branch is located on Danielson Pike, near the Connecticut line.
“Like here in Burrillville,” Bancroft said, “out there we are the only provider in the community — the only primary care, dental and behavioral-health care in Foster. And there, we’re seeing about 30% of the town. So again, we’re responding to community needs.”
The same is true, he said, for WellOne’s two other locations.
Several centers serve rural areas
Other centers that serve rural populations include Thundermist Health Center, which has an office in South County; Block Island Health Services, which serves New Shoreham; and Wood River Health Services, with offices in Hope Valley and Westerly for people living in southwestern Rhode Island.
Wood River president and CEO Alison L. Croke wrote in an email that the center “was founded in 1976 to meet the needs of a community with limited access to convenient, high-quality health care services. Many of our community members’ health care needs are compounded by food insecurity, housing challenges and lack of transportation. For these individuals, and for our community as a whole, Wood River serves as a lifeline.”

Last year, according to Croke, Wood River, with its staff of 89, served 7,146 patients. “This represents 20,347 primary-care visits, 4,780 dental visits and 1,146 behavioral-health visits,” she said. The center, she added, is in a federally designated Health Professional Shortage Area, “and this lack of access highlights the need for our services to exist in the community.”
United Way wants to raise $4.01 million for nonprofits as 401Gives returns
Like WellOne, the needs of some of Wood River’s patients transcend medial, dental and behavioral-health care, Croke said.

“Transportation is a large barrier to care in our community, and we have a community fund to assist patients that need help with this as well as other social determinants,” she wrote. “The biggest emerging issue we see now with our patients (as well as our staff) is the fear of losing housing and the affordability of housing.”
Steering through a pandemic
More than a century after a nurse in a borrowed horse and buggy tended to rural Rhode Islanders during the tuberculosis pandemic, the center she founded persevered through the COVID pandemic.
“During the early stages,” Bancroft said, “our primary-care services were transitioned to a virtual service delivery model for about 80% of patient visits. In-office primary care visits resumed during the second half of the pandemic.”
State health officials:Will Rhode Island see another COVID-19 spike this spring?
During the first month of the pandemic, Bancroft said, “dental services were substantially suspended with the exception of emergency services” to comply with state Health Department and CDC requirements. “These services resumed in July 2020 with new infection control measures in place. Our behavioral-health services transitioned to a virtual platform at the onset of the pandemic.”
They are still provided virtually, Bancroft said.
Staff devotion
Services continued with cooperation of staff, including nurse practitioner Joan K. Mullaney, who began work in 1979 at a center that would become WellOne. During a recent interview in the wing where she provides primary care, she recalled a location that today is the myriad of medical, dental and administrative offices along Bridge Way and Sayles Avenue.
“This building was literally a little brick building with, like, three little exam rooms,” she said. “It was just this tiny building. It’s expanded so much.”

A resident of Glocester, Mullaney said she was drawn to the center — and has stayed more than four decades — by her love of rural communities and her ability to meet the health needs of residents who cannot or choose not to travel to the cities. Particularly satisfying, she said, is becoming familiar with generations of families.
“I get to know my patients,” she said, and because she doesn’t keep her eye on the clock, “I run late all the time.”
Nearly 9 in 10 rural Vermonters:New funding supports 11 community health centers
Some visits lengthen because of “chit-chat,” she said, but others for reasons beyond friendship. “It might be a patient needs extra time during a crisis — somebody died in the family or they lost a pet. One of my patients lost her horse and she just sobbed away and I was practically crying with her.”
Mullaney added: “I’m helping people. I was meant to be a caregiver.”
‘Serving a community’
WellOne dental assistant Brooke Casey grew up in Foster, graduated in 2014 from Ponaganset High School, and after completing dental assisting study and training, took a job in Providence. But then she had a baby and wanted employment that was “more fit for being a mom” — a job with flexibility, good benefits and a short commute.
A patient of WellOne while she was growing up, Casey decided to apply there, and in June 2020 she was hired. She has two young children now and lives in Chepachet.
“I like serving a community,” she told The Journal. “We’re able to help people, and that’s a huge thing. So is being able to put my foot forward and help people where they need it.”

Casey traces her commitment to her childhood.
“I was adopted as a very, very young child, so it kind of starts there,” she said. “My adoptive parents took a jump in their lifestyle to help kids in need. My mom was always a stay-at-home mom, but she was a foster parent for many, many years. My dad was a full-time electrician until he retired. Now, they’re at home. Growing up with them made me a passionate, caring person looking to help others.”
Hoping to swim and kayak again
The sun sparkled across Wakefield Pond as Jim Whiteside discussed the hard decision he made recently to sell his truck, now that he can no longer drive — and his transportation these days, a WellOne wheelchair van, “which is great for people like me. They will even take you to places other than even WellOne.”
“I’m at least an hour and 10 minutes from Providence. You really can’t go any much further north and west in the state. From what I hear from the nurses [who] come up to visit me, there are quite a few other patients they have up here. If it wasn’t for WellOne and a couple of other services, I wouldn’t be able to remain in my home. I’d have to live someplace else and I don’t want to do that. This is where I want to be.”

As the interview wound down, Whiteside outlined his ambitions for this summer.
“I’m dying to go in the water,” he said. “After I had my leg taken off, I went in twice, but it wasn’t a good thing because I didn’t know how to swim anymore. I grew up swimming. But how do you swim with one leg? I really want to learn. I’ll get the life preserver and I’ll put that on and learn.”
And once he does, he aims to go boating in his new kayak.
Last year, he said, “I tried a couple of times. I was going around the shore but I kept tipping over because I didn’t have the leg on and there was more weight on one side. I said ‘if I tip over out in the middle of the lake, I’m going to the bottom. So I’ve got to figure out how to do it. And I will.”
